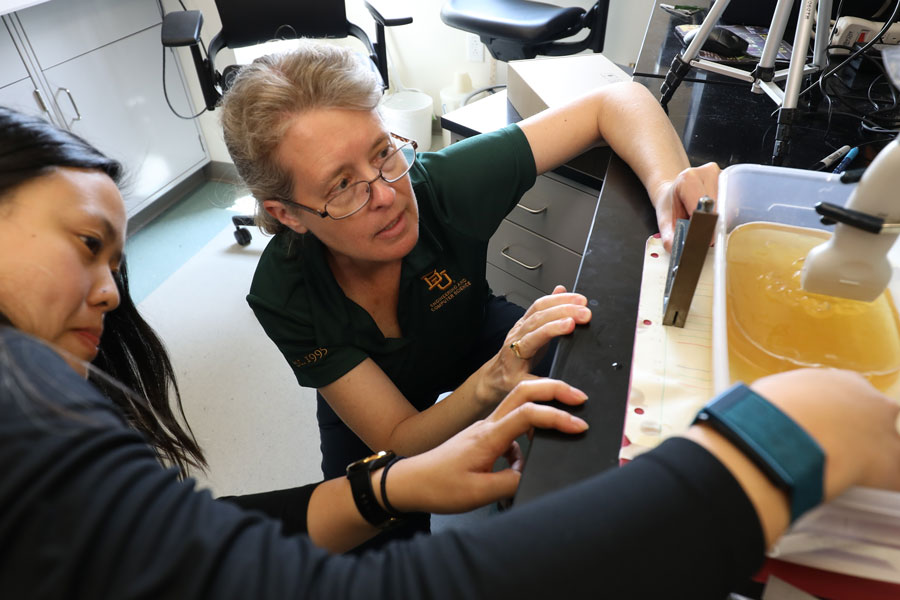
Dr. Linda Olafsen
Baylor Researchers Uncovering Improved Approach to Treat Internal Injury
On the battlefield, a medic reaches an injured soldier suffering from a traumatic injury. Locating and treating the source of internal bleeding is difficult, however, hindering efforts to stabilize the soldier for transport. Elsewhere, at a VA hospital, a military veteran undergoing surgery is at high risk for stroke or aneurysm. The hospital requires better options to monitor health and immediate intervention to prevent permanent brain damage.
These are just two of the many real-world issues that a team of researchers led by Linda Olafsen, Ph.D., associate professor of electrical & computer engineering, is addressing through an interdisciplinary approach combining infrared sensing and ultrasound imaging within the human body, resulting in a wire that can help medical practitioners find where an injury took place.
“We’re working on devices that can help locate the injury so it can be identified, embolized, controlled and stabilized in order for soldiers to safely make that longer trip to a more comprehensive treatment facility,” Olafsen says.
Programmable, Malleable Internal Navigation
The interdisciplinary approach brings together experts in fields like medicine, materials science, electrical engineering and physics. Seven team members are from Baylor University, including Keith Schubert, Ph.D., professor of electrical & computer engineering, and Jeffrey Olafsen, Ph.D., associate professor of physics. Collaborators from outside Baylor represent Johns Hopkins University School of Medicine, Anne Arundel Health System (Annapolis, MD), Baylor Scott & White Health Neuroscience Institute and Texas A&M University College of Medicine.
“Here at Baylor, we’re very interested in materials science, including the programmable wire that we’re using to navigate inside the human body,” Olafsen says. “Our engineering and science skills in partnership with medical colleagues’ knowledge helps us better design and evaluate products and applications. It’s great that we can engineer this wire and control it to bend on command, but can a doctor actually use it? The interdisciplinary approach allows us to achieve engineering solutions that are useful to entities like the Department of Defense. It’s collaboratively designed to help save lives.”
A crucial component of the research involves surgical wire that can be used to navigate arteries to find and stop internal bleeding, cauterize wounds, and monitor blood oxygen levels, chemical levels, or tumor growth. The wire is a biosafe product called Nitinol, a nickel-titanium alloy originally developed at the Naval Ordnance Laboratory. While Nitinol has been around for decades, Olafsen’s team has created a new application and scaled down its size.
“The wire, a shape-memory alloy, is malleable,” Olafsen explains. “By heating the wire to a certain temperature, we’re able to activate it and remind it of a particular shape. That will cause the wire to bend. So, when you’re navigating through an artery and reach a branch, you apply a current, and that will allow the wire to bend, and then you can turn the current off so that the wire follows the artery. When you reach another bend, you can again apply a current and make the next turn.”
Meeting Practical Medic Needs
“The more we can scale down, the more options we have to put devices at the end of these wires for specific applications. If I want to put one of my infrared emitters at the tip of a 100-micrometer wire, we’re going to have to go down to micro-LED scales. Arteries to the heart are pretty large, but if we want to navigate up into the brain to treat an aneurysm, then we’re going to have to go to smaller. That creates fun materials and engineering challenges to solve.”
The group is interested in developing materials and biomedical devices that can be operated in safe wavelength ranges for sensitive chemical detection. The ability to sense infrared wavelengths will not only help the diagnosis and treatment of traumatic brain injury and neuro conditions but also can be used to help monitor the heart, liver, spleen, spine and other areas with enhanced specificity and sensitivity.
Olafsen says the initial endovascular navigation project grew from conversations with physicians at Baylor Scott & White Health in Temple who are interested in finding more effective ways to treat aneurysms and neurovascular conditions. The team looks at creating practical, efficient solutions that work in a controlled environment like a hospital and in the field, where conditions are much less predictable.
A medic needs a device that is easy to power, easy to operate and easy to transport, says Olafsen, who previously worked with the U. S. Naval Research Laboratory to develop infrared devices. That work has been supported by the Air Force Office of Scientific Research as well as by an Office of Naval Research Young Investigator Award.
“I love being able to help our soldiers and our country, and I love being able to apply my physics, engineering and semiconductor knowledge to things that matter, providing the military with technology that’s going to help save our soldiers and improve the quality of life of our veterans,” Olafsen says.
In the future, Olafsen anticipates opportunities to apply this technology to telemedicine and remote surgery.
“We’re very excited to develop a robotic or voice-activated system,” she says. “You could have a remote controlled system or even very remote observation to enable a knowledgeable surgeon on a different continent to help during treatment, depending on which devices we have attached to the end of our endovascular navigation system.”